Wish To Do More In Ebola Fight Meets Reality In Liberia
November 2, 2014 - By Sheri Fink - New York Times

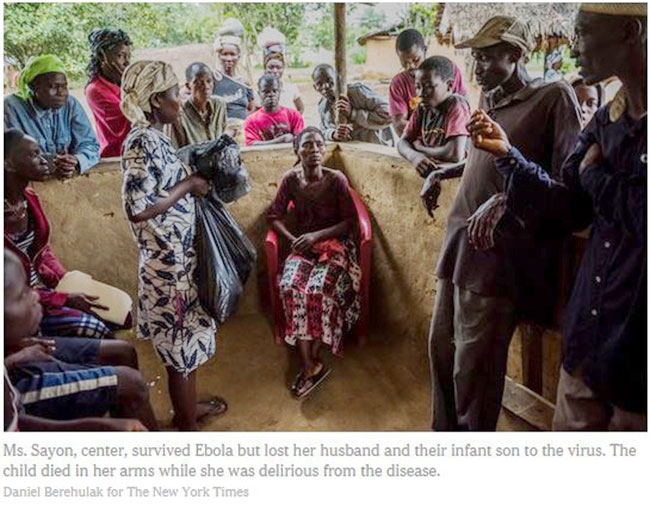
SUAKOKO, Liberia — Garmai Sayon endured more than anyone should have to bear. First, her husband died at the Ebola treatment center here, falling ill after rushing to help a stranger who had collapsed in their village. Five days later, their child — a 1-year-old boy whose two older siblings had been lost earlier to illness and accident — died in her arms while she was delirious from the disease.
Doctors and nurses tended to the young woman as she had fevers, suffered pains all over her body and lay listless, confused. “I just gave my heart to God,” Ms. Sayon recalled.
As her symptoms began to abate, her arm grew hot and swelled to twice its size, prompting fears of sepsis, an often deadly complication of infection. It most likely stemmed from where her intravenous line had been inserted but not changed as often as desirable because of risks, both to her and to the medical workers. Ms. Sayon had survived Ebola, but it was not yet certain that she would survive the treatment.
What level of care is possible for a disease with no cure being treated in wooden huts in the middle of a forest? How do medical workers prioritize which patients and tasks to focus on when they cannot do everything they were trained to do? Will their decisions determine who lives and who dies? And how would they even know?
“You always want to do more, but it has to be balanced with what’s possible, with what makes sense for the context you’re working in,” said Dr. Pranav Shetty, the medical director at the center operated here by International Medical Corps.
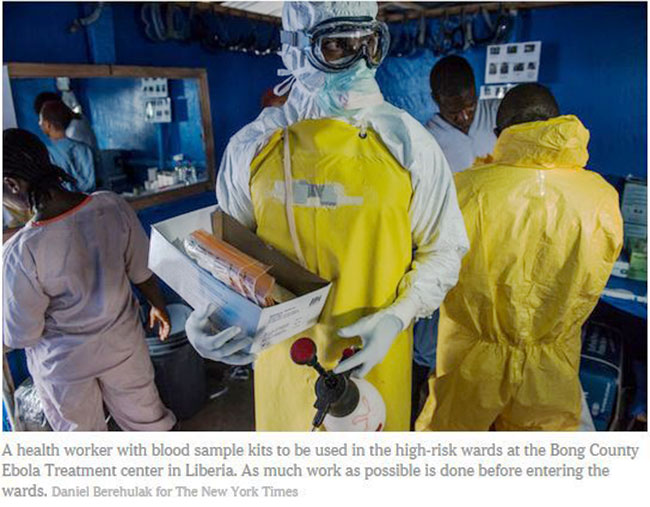
Because of the limited time they can spend in the sick wards in their stifling protective suits, the risks of certain procedures and even the amount of medicines available, health workers here and elsewhere in West Africa ration care, operating under constraints they often find frustrating. The mainstays of fighting the Ebola epidemic — isolation and basic treatment — have resulted in more dead than survivors among those infected, just like with Ms. Sayon’s family.
Nurses and doctors here improvise, taking small steps in hopes of improving the odds. They tie ropes to the rafters to hang IVs, then use blood-pressure cuffs to squeeze the bags of fluids into patients faster. Doctors prescribe a regimen of antibiotics and antimalarial medications to treat every patient for possible other illnesses coexisting with Ebola, because they do not have access to tests for them. “It’s surprising how much you can do without,” said Dr. Steve Whiteley, an emergency medicine doctor from California, one of six physicians currently on rotation here.
But, he said, that is not nearly enough. So far, the clinic’s record appears similar to that of other treatment facilities in the countries hit hard by Ebola. From mid-September, when the clinic opened, to Monday morning, 36 patients who tested positive for the disease died; 21 recovered; and others remained in treatment. Its fatality rate of 63 percent could change, as such measures tend to fluctuate.
Like others who have fought the disease close up, Dr. Whiteley and some colleagues here are pressing for more aggressive action. They are combing patient data for clues to what factors correlate with survival, and studying best practices with other treatment centers. They are debating everything from whether the center should install cooling systems, which might reduce dehydration among patients, to performing bedside testing and other interventions. Those could include experimental treatments, which the aid group Doctors Without Borders announced recently it would begin studying.
“We help fewer than half, if help means save,” Dr. Whiteley said. “We do a lot, but we need to do more.”
Treatment Perils
In the treatment wards, some of medicine’s most basic tools are hard to use. With their heads wrapped in protective coverings, the doctors and nurses do not use a stethoscope to listen for heart or breath sounds. Manual blood-pressure measurements present similar problems. Their hands sheathed in three pairs of gloves, the medical workers often struggle to find a vein by touch in order to draw blood. They do not keep detailed patient charts in the steamy wards — it is damp and difficult to see through fogged goggles — or remove notes because they would have to be disinfected.
The single lab test performed on patients here, a high-tech analysis that detects the virus, proved troublesome in the clinic’s first two weeks. A blood sample from Ms. Sayon, 23, for example, was drawn Sept. 28, the day after her arrival, but was lost after being handed over for shipment to a lab in the capital, Monrovia, more than four hours away. That experience was not uncommon, workers at the center said. Ms. Sayon was retested five days later, after a mobile Ebola detection laboratory of the United States Navy opened near the treatment center, cutting from days to hours the time required for a diagnosis.
“Is she the one who lost her baby and husband?” Dr. Steven Hatch, a volunteer from Worcester, Mass., asked during rounds one day at a whiteboard outside the wards, where staff members gathered after being sprayed down with a bleach solution and removing their protective suits. They wrote brief notes from memory about their patients.

The medical team later discussed the possibility of bringing scanners to copy and send notes from inside the wards, or using walkie-talkies to relay information to those outside. “It’s too hard to keep track of all the patients in your head,” Dr. Whiteley said.
He and others often rely on their instincts and experience. When Ms. Sayon’s second blood test for Ebola came back, the results were negative, but the doctors were wary of releasing her. She was bent over in a chair, shaking. Her eyes and cheeks were sunken. Keeping her in the ward for suspected cases risked infecting her with the virus, but the physicians reasoned she already had significant exposure from her family, and virus detection can sometimes lag symptoms by up to three days. (They also suspected there might have been a mix-up because of labeling problems that day with blood samples that the new center quickly worked to fix.)
“Solomon would be on his knees after a week here,” Dr. Hatch said. “Every day there’s a new dilemma we haven’t considered.”
The risk-benefit calculus shapes almost everything. Before going into the treatment wards, one physician recently proposed setting clear priorities and one-hour limits. Drawing blood is vital, so Colin Bucks, an emergency doctor from Stanford, improvised tube holders to make the process safer. Doctors and nurses operate blindly at times, so they are seeking more diagnostic tools. Some staff members cheered Wednesday when Dr. Patricia Henwood, an emergency medicine specialist at the University of Pennsylvania volunteering here, announced that she hoped to get a portable ultrasound machine through a nonprofit she helped found. If one had been here already, doctors might have quickly ruled out a blood clot as the cause of Ms. Sayon’s swollen arm and been more certain that treating her with antibiotics for a possible life-threatening infection was the correct course.
The center dispenses drugs to alleviate Ebola symptoms, including anti-nausea medicine, a Tylenol-like painkiller that reduces fever and Haldol, an antipsychotic medication for patients writhing in delirium. It also has a team of mental health professionals who provide counsel and comfort. (The center’s first movie night, with “The Lion King” projected on a sheet outdoors, drew even some of the sickest patients last week.)
A nurse gave a generic version of the sedative Valium to Ms. Sayon when she was feverish and appeared depressed. But with some supply shortages, staff members try to be prudent. “You have to be conscious of not just throwing everything at everyone,” Dr. Henwood said. If the center ran out of the sedative, and it was needed for a patient suffering a prolonged seizure, “You wouldn’t have medicine for them.”
For several patients who seemed in agony, one doctor said he might have considered intravenous morphine. But International Medical Corps, a charity based in Los Angeles, has not completed the requirements set by Liberian authorities to administer the narcotic painkiller. Even if they could dispense it, several of the doctors were wary. Patients who were desperately ill sometimes made surprising recoveries, they warned, and too much morphine, which can depress breathing, could lead to an unnecessary death.
Perhaps the most potent tool the doctors and nurses have available for patients who cannot keep down liquids are IV fluids, to combat dehydration that can set off a deadly cascade: low blood pressure, electrolyte imbalances and organ failure. IV lines, though, pose certain risks. They require a needle, which can endanger health workers, and the insertion site should be changed frequently, which can harm Ebola patients vulnerable to bleeding. Also, the bag of fluids and the tubing are being removed when no nurses or doctors are present to prevent injury if a patient dislodges the apparatus. Like many others at the center, Ms. Sayon had begun receiving IV fluids soon after her arrival.
“It would just be nice to have a better gauge of who needs it and how much,” said Dr. Whiteley, who practices at Kaiser Vallejo in Northern California. “I’d like to have more to go on than an educated guess.”